What Male Reproductive Services Are Covered By Health Insurance
| Central Takeaways |
|
Introduction
Many people require fertility assistance to have children. This could either exist due to a diagnosis of infertility, or because they are in a same-sex relationship or single and desire children. While at that place are several forms of fertility help, many services are out of reach for almost people because of price. Fertility treatments are expensive and often are not covered by insurance. While some private insurance plans cover diagnostic services, there is very niggling coverage for handling services such every bit IUI and IVF, which are more expensive. Virtually people who use fertility services must pay out of pocket, with costs oftentimes reaching thousands of dollars. Very few states require individual insurance plans to cover infertility services and only ane state requires coverage under Medicaid, the health coverage programme for depression-income people. This widens the gap for low-income people, even when they take health coverage. This brief examines how access to fertility services, both diagnostic and treatment, varies beyond the U.Due south., based on country regulations, insurance type, income level and patient demographics.
Diagnosis and Handling Services
Infertility is almost commonly divers1 as the inability to achieve pregnancy later ane year of regular, unprotected heterosexual intercourse, and affects an estimated 10-15% of heterosexual couples. Both female and male person factors contribute to infertility, including issues with ovulation (when the ovary releases an egg), structural problems with the uterus or fallopian tubes, problems with sperm quality or motility, and hormonal factors (Effigy 1). About 25% of the time, infertility is caused by more than than one factor, and in well-nigh 10% of cases infertility is unexplained. Infertility estimates, yet exercise not account for LGBTQ or single individuals who may also demand fertility aid for family unit edifice. Therefore, there are varied reasons that may prompt individuals to seek fertility care.

Figure 1: There Are Multiple Reasons Someone May seek Fertility Assist
A broad array of diagnostic and treatment services may be necessary to aid in fertility (Tabular array 1). Diagnostics typically include lab tests, a semen assay and imaging studies or procedures of the reproductive organs. If a likely cause of infertility is identified, treatment is ofttimes directed at addressing the source of the problem. For instance, if someone has abnormal thyroid hormone levels, thyroid medications may help the patient achieve pregnancy. If a patient has large fibroids distorting the uterine cavity, surgical removal of these benign tumors may allow for time to come pregnancy. Other times, other interventions are needed to help the patient accomplish pregnancy. For example, if a semen assay reveals poor sperm move or the fallopian tubes are blocked, the sperm volition not be able to fertilize the egg, and intrauterine insemination (IUI) or in-vitro fertilization (IVF) may be necessary. These procedures as well facilitate family building for LGBTQ and single individuals, with use of donor egg or sperm, with or without a gestational carrier (surrogacy).
| Table 1: Overview of Common Fertility Services | |
| Diagnostic Services: |
|
| Treatment Services: |
|
| Fertility Preservation: |
|
| NOTES: This is non an exhaustive list of infertility services. SOURCE: ACOG. Evaluating Infertility. 2017; ACOG. Treating Infertility. 2019; American Society for Reproductive Medicine. Infertility: An Overview. Patient Information Series. 2017 | |
Utilization of Fertility Services
Our analysis of the 2015-2017 National Survey of Family Growth (NSFG) finds that x% of women2 ages xviii-49 say they or their partner have ever talked to a doctor near ways to help them become meaning (data not shown).3 Among women ages eighteen-49, the nigh ordinarily reported service is fertility advice (Figure 2).
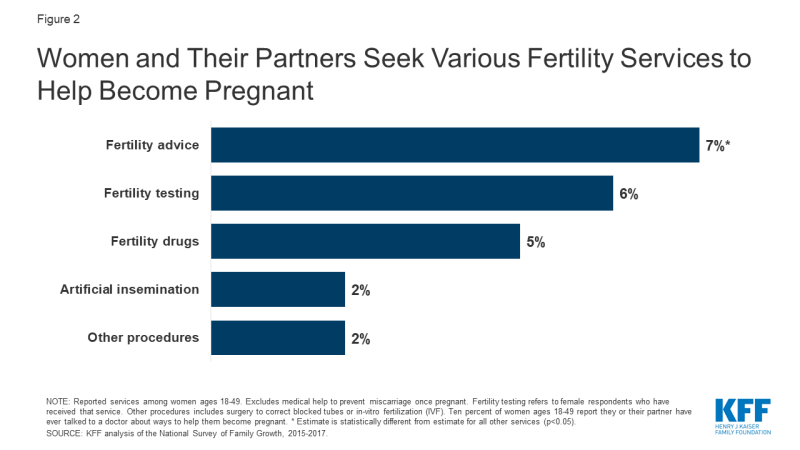
Effigy 2: Women and Their Partners Seek Various Fertility Services to Assistance Become Meaning
The CDC finds that use of IVF has steadily increased since its showtime successful birth in 1981. According to the almost recent data, an estimated ane.viii% of U.S. infants are conceived annually using assisted reproductive technology (ART) (e.g., IVF and related procedures).4 The proportions are highest in the Northeast (MA 4.7%, CN iii.9%, NJ three.9%), and lower in the South and Southwest (NM 0.iv%, AR 0.half dozen%, MS 0.half-dozen%).
Utilization of fertility services has dropped drastically during the COVID-nineteen public health emergency. On March 17, 2020 the American Order for Reproductive Medicine (ASRM) issued guidelines to stop all new fertility treatment cycles and not-urgent diagnostic procedures. Since then, ASRM has provided updated guidance on what weather should exist met and measures should be taken before safely resuming fertility care. During this time, a report by Strata Decision Engineering science of 228 hospitals across 40 states found patient encounters for infertility services were down 83% from March 22 to April 4, 2020 compared to this time the year prior.
Cost of Services
Many patients lack admission to fertility services, largely due to its high cost and limited coverage by private insurance and Medicaid. As a result, many people who apply fertility services must pay out of pocket, even if they are otherwise insured. Out of pocket costs vary widely depending on the patient, state of residence, provider and insurance plan. By and large, diagnostic lab tests, semen analysis and ultrasounds are less expensive than diagnostic procedures (e.g., HSG) or surgery (e.g., hysteroscopy, laparoscopy). Meanwhile treatment using fertility medications is less expensive than IUI and IVF, simply even the less costly treatments tin can nevertheless result in thousands of dollars of out of pocket costs. Many people must attempt multiple treatments before they or their partner tin can achieve a pregnancy (typically medication first, followed by surgery or fertility procedures if medications are unsuccessful). A study of most 400 women undergoing fertility care in Northern California demonstrates this overall trend, with the lowest out of pocket spending on treatment with medication simply and the highest costs for IVF services (Figure 3). Prior research showed the cost of just 1 standard cycle of IVF was approximately $12,500 in 2009, just is likely higher today due to rising wellness care costs overall. Furthermore, many patients crave several rounds of treatment before achieving a pregnancy, with costs accruing each bike making these interventions financially inaccessible for many. In addition to costs for the bodily treatment, patients can be saddled with out of pocket expenses for office visits, diagnostic tests/procedures, genetic testing, donor sperm/egg apply and storage fees and wages lost from time off piece of work.
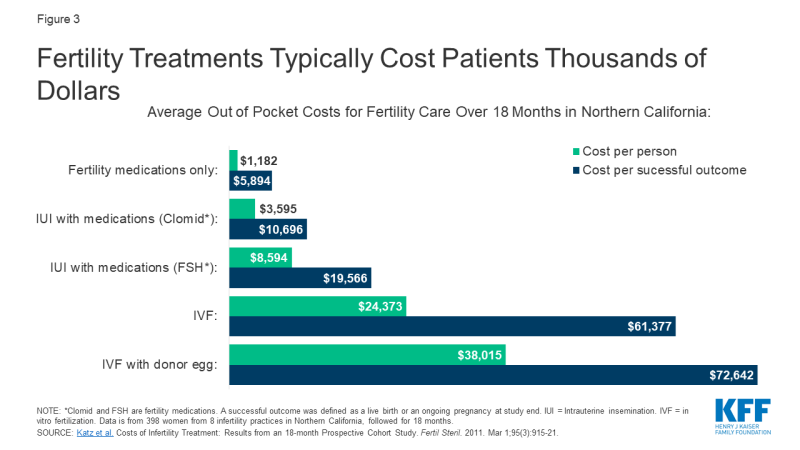
Figure 3: Fertility Treatments Typically Cost Patients Thousands of Dollars
Insurance Coverage
Insurance coverage of fertility services varies by the state in which the person lives and, for people with employer-sponsored insurance, the size of their employer. Many fertility treatments are non considered "medically necessary" by insurance companies, then they are non typically covered by private insurance plans or Medicaid programs. When coverage is bachelor, certain types of fertility services (e.one thousand., testing) are more likely to be covered than others (e.g., IVF). A handful of states require coverage of fertility services for some fully-insured private plans, which are regulated past the state. These requirements, however, do not apply to health plans that are administered and funded directly by employers (cocky-funded plans) which cover six in ten (61%) workers with employer-sponsored wellness insurance. States also have purview over the benefits covered by their Medicaid programs. The federal government has authority over benefit requirements in federal health coverage programs, including Medicare, the Indian Health Service (IHS) and military health coverage.
Private Insurance
Xv states have laws in effect requiring certain health plans to encompass at least some infertility treatments (a "mandate to cover") (Figure 4). Additionally, Colorado recently enacted a requirement for private and group wellness do good plans to cover infertility diagnosis, handling and fertility preservation for iatrogenic infertility, effective January 2022. Among states that practice not have a mandate to cover, nine states5 and DC have a benchmark programme that includes coverage for at to the lowest degree some infertility services (diagnosis and/or treatment) for most individual and small group plans sold in that state.half dozen Two states (CA and TXseven) require group health plans to offering at to the lowest degree one policy with infertility coverage (a "mandate to offer"), but employers are not required to choose these plans.
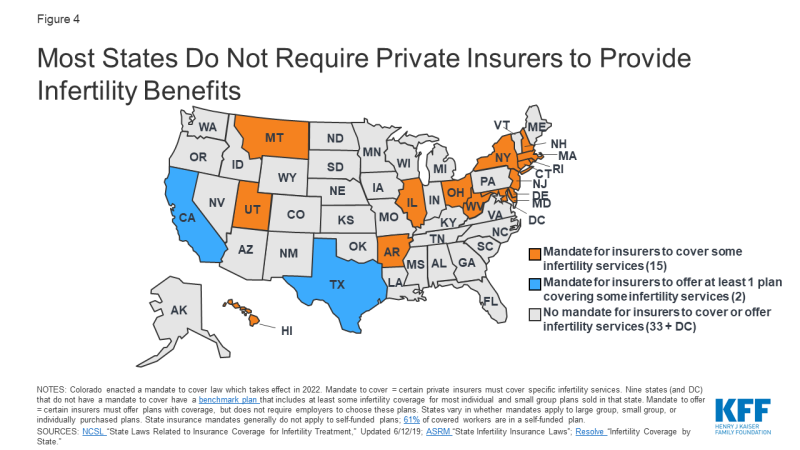
Figure 4: Most States Do Not Require Individual Insurers to Provide Infertility Benefits
However, in states with "mandate to cover" laws, these only apply to certain insurers, for sure treatment services and for sure patients, and in some states have monetary caps on costs they must cover (Appendix one). For example, in OH and WV, the requirement to cover infertility services but applies to health maintenance organizations (HMOs). In other states, almost all insurers and HMOs are included in the mandate. Many states provide exemptions for small employers (<50 employees) or religious employers. In improver, land laws do not utilize to self-funded (or self-insured) employer plans, which are regulated past federal law. Threescore-one percentage of covered workers are enrolled in a self-funded programme.
Even in states with coverage laws, non all patients are eligible for infertility treatment. In How-do-you-do, someone with unexplained infertility only qualifies for IVF after five years of infertility. In others, patients are eligible afterwards 1 year. Some states place age limits on female patients who can access these services (e.1000., ineligible if 46 or older in NJ or if under age 25 or older than 42 in RI). Others place restrictions based on marital status; for example, until May 2020, IVF benefits were only bachelor to married women in MD. Recently enacted legislation at present expands coverage to single women. Additionally, it is not ever made clear if LGBTQ individuals run across eligibility criteria for these benefits, without a diagnosis of infertility. Furthermore, many costs associated with surrogacy are often non covered by insurance.
States also vary in which treatment services they require plans to cover. Some states mandate insurers to comprehend cryopreservation for persons with iatrogenic infertility, while others do non. 4 states with insurer mandates do non cover IVF. Eleven states do, merely with a dollar limit on coverage (east.g., $15,000 lifetime max in AR and $100,000 in MD and RI) or a limit on the number of cycles they volition encompass (e.g., ane cycle of IVF in HI and 3 cycles in NY).
Do state mandates for IVF coverage affect use of services?
IVF utilization appears to be higher in states with mandated IVF coverage. CDC data from 2016 showed that in iii of the four states deemed by the CDC to have "comprehensive coverage"8 for IVF (IL, MA, NH), utilise of assisted reproductive engineering science was i.5 times college than the national rate. Similarly, a national study found that IVF availability and utilization9 were significantly higher in states with mandated IVF coverage. A written report in MA found IVF utilization increased after implementation of their IVF mandate, but overutilization by patients with a depression chance of pregnancy success was non found. State level mandates can also help reduce inequities in admission. For example, a recent neb proposed in the CA legislature would contrary existing limitations on fertility coverage and make the benefit available to single women and women in aforementioned sex relationships.
What does information technology price to cover fertility benefits?
While the costs of fertility treatments can be very expensive for those who lack coverage, the price of covering fertility benefits varies depending on the services covered and utilization with implications for state budgets, employers, and policy holders. For example, in 2019, New York passed a bill to require IVF and fertility preservation services for comprehensive individual health insurance policies. The New York State Department of Financial Services estimated that premiums would increase 0.v% to one.one% due to mandating IVF coverage, and 0.02% for mandating fertility preservation for iatrogenic infertility (caused by medical treatments).
An assay of a bill proposed in CA to require private plans and Medi-Cal managed care plans to encompass IVF services estimated that per member per month premiums would increase past approximately $5 in the private market and less than a $ane.00 for Medi-Cal plans. Overall though, out of pocket spending for individuals seeking services would decrease substantially.
Data from MA, CT and RI suggest that mandating coverage does not appear to heighten premiums significantly. All three states accept been mandating infertility benefits for over thirty years, and estimate the toll of infertility coverage to exist less than 1% of full premium costs. In 2017, California was because a more than limited beak that would require fertility preservation for iatrogenic infertility in certain individual and group wellness plans. As the bill was introduced, it was estimated to effect in a net annual increase of $2,197,000 in premium costs or 0.0015% for enrollees in plans subject to the mandate.
While these costs could exist modest in comparing to the costs of paying out-of-pocket for these services, in that location are other costs to coverage mandates. The ACA requires states to offset some of the costs for whatever country mandated benefits beyond essential health benefits (EHBs) in the individual and small group market. This requirement was estimated to cost NY $59 to $69 million per year if covering one cycle or $98 to $116 million per year if roofing unlimited cycles of IVF.
What share of employers offering fertility benefits?
Large employers are more than likely than smaller employers to include fertility benefits in their employer-sponsored health plans. According to Mercer'due south 2017 National Survey of Employer-Sponsored Health Plans, 56% of employers with 500 or more employees cover some type of fertility service, merely most practise non encompass handling services such as IVF, IUI, or egg freezing. Coverage is higher for diagnostic evaluations and fertility drugs. Coverage is more than mutual amidst the largest employers and those that offer higher wages (Figure 5).
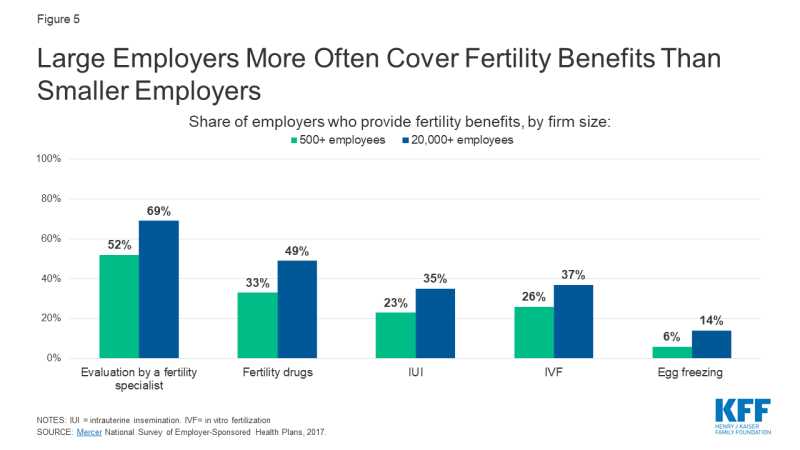
Figure 5: Big Employers More Often Comprehend Fertility Benefits Than Smaller Employers
Public Coverage
Medicaid
NSFG data evidence that significantly fewer women with Medicaid have e'er used medical services to assistance go pregnant compared to women with private insurance. As of Jan 2020, our analysis of Medicaid policies and benefits reveal just one state, New York, specifically requires their Medicaid program to cover fertility treatment (limited to 3 cycles of fertility drugs) (Figure 6). Yet, some states may crave Medicaid to cover treatments for conditions that touch on fertility, while not direct stated in their policies. For example, states may cover thyroid medications, or cover surgery for fibroids, endometriosis or other gynecologic abnormalities if causing pelvic pain, aberrant bleeding or another medical problem, other than infertility. No state Medicaid program currently covers artificial insemination (IUI), IVF, or cryopreservation (Appendix ii).
Some states specifically cover infertility diagnostic services; GA, HI, MA, MI, MN, NH, NM and NY all offering at least one Medicaid plan with this do good, merely the range of diagnostics covered varies. For instance, New York Medicaid specifically covers office visits, HSGs, pelvic ultrasounds and blood tests for infertility. Meanwhile, the infertility assessment covered by Georgia Medicaid includes lab testing, but not imaging or procedural diagnostics. Other states specifically practise not comprehend infertility diagnostics, or more generally do not embrace "infertility services," which likely includes diagnostics. Others do not mention infertility diagnostics in their Medicaid policies, meaning the beneficiary would need to check with their Medicaid program to run across if these services are covered (Appendix two).
The Medicaid program'south lack of coverage of fertility assistance has a disproportionate impact on women of colour. Among reproductive age women, the program covers three in ten (30%) who are Black and i quarter who are Hispanic (26%), compared to 15% who are White. Because eligibility for Medicaid is based on being low-income, people enrolled in the program likely could not afford to pay for services out of pocket.
The relative lack of Medicaid coverage for fertility services stands in stark contrast to Medicaid coverage for motherhood care and family unit planning services. Nearly half of births in the U.South. are financed by Medicaid, and the program finances the majority of publicly-funded family planning services. Therefore, while there is broad coverage of many services for low-income people during pregnancy and to aid preclude pregnancy, there is almost no access to help low-income people achieve pregnancy.

Figure 6: One State Medicaid Program Covers Infertility Treatment and 8 Cover Some Diagnostics
Medicare
While almost beneficiaries of Medicare are over the historic period of 65+, Medicare likewise provides health insurance to approximately ii.five million reproductive age adults with permanent disabilities. According to the Medicare Benefit policy manual, "reasonable and necessary services associated with treatment for infertility are covered nether Medicare." Still, specific covered services are not listed, and the definition of "reasonable and necessary" are not divers.
Military
TRICARE: TRICARE, the insurance program for war machine families, will cover some infertility services, if deemed "medically necessary" and if pregnancy is achieved through "natural conception," meaning fertilization occurs through heterosexual intercourse. Diagnostic services are covered, including lab testing, genetic testing, and semen assay. Treatment to correct physical causes of infertility are also covered. However, IUI, IVF, donor eggs/sperm and cryopreservation are not typically covered, unless the service member had a serious injury while on active duty resulting in infertility.
Veterans Diplomacy (VA): Infertility services are covered by the VA medical benefits package, if infertility resulted from a service-connected condition. This includes infertility counseling, blood tests, genetic counseling, semen analysis, ultrasound imaging, surgery, medications and IVF (equally of 2017). Yet, the couple seeking services must exist legally married, and the egg and sperm must come up from said couple (effectively excluding same sex couples). Donor eggs/sperm, surrogacy or obstetrical intendance for non-Veteran spouses are non covered.
Infertility Services In Publicly Funded Clinics
The CDC's and Role of Population Diplomacy' (OPA) Quality Family unit Planning recommendations accost provision of bones infertility services. Family planning providers are recommended to provide at minimum patient teaching virtually fertility and lifestyle modifications, a thorough medical history and physical exam, semen analysis, and if indicated, referrals for lab testing of hormone levels, boosted diagnostic tests (endometrial biopsy, ultrasound, HSG, laparoscopy) and prescription of medications to promote fertility. All the same, studies of publicly funded family planning clinics suggest that availability of infertility services is uneven. In a 2013-2014 study of 1615 publicly funded clinics, a high share reported offer preconception care (94% for women and 69% for men), simply fewer offered whatsoever basic infertility services (66% for women and 45% for men). Provision of any infertility handling was uncommon (xvi% of clinics), likely requiring referrals to specialists who may not accept Medicaid or uninsured patients.10 The majority of patients who rely on publicly funded clinics are low-income and would non probable be able to afford infertility services and treatments once diagnosed.
Per the Indian Health Services (IHS) provider manual, basic infertility diagnostics should exist made available to women and men at IHS facilities, including a history, concrete examination, basal temperature charting (to predict ovulation), semen analysis and progesterone testing. In facilities with OBGYNs, HSG, endometrial biopsy and diagnostic laparoscopy should also be available. Even so, it is unclear how attainable these services are in practise, and provision of infertility treatment is not mentioned.
Fundamental Populations
Racial and indigenous minorities
The ability to have and care for the family unit that you wish for is a fundamental tenet of reproductive justice. For those who need it, this includes admission to fertility services. The share of racial and ethnic minorities who utilise medical services to help become significant is less than that of non-Hispanic White women, despite research that has found higher rates of infertility among women who are Blackness and American Indian / Alaska Native (AI/AN). Our analysis of 2015-2017 NSFG data shows that while 13% of non-Hispanic White women reported ever going to a medical provider for assist getting pregnant, only vi% of Hispanic women and 7% of non-Hispanic Black women did and then (Figure seven). A higher share of Black and Hispanic women are either covered past Medicaid or uninsured than White women and more women with private insurance sought fertility assist than those with Medicaid or the uninsured. A multifariousness of factors, including differences in coverage rates, availability of services, income, and service‐seeking behaviors, affect access to infertility care. Furthermore, other societal factors also play a role. Misconceptions and stereotypes about fertility have often portrayed Black women equally not requiring fertility assistance. Combined with the history of discriminatory reproductive care and impairment inflicted upon many women of color over decades, some may delay seeking infertility care or may not seek information technology at all.
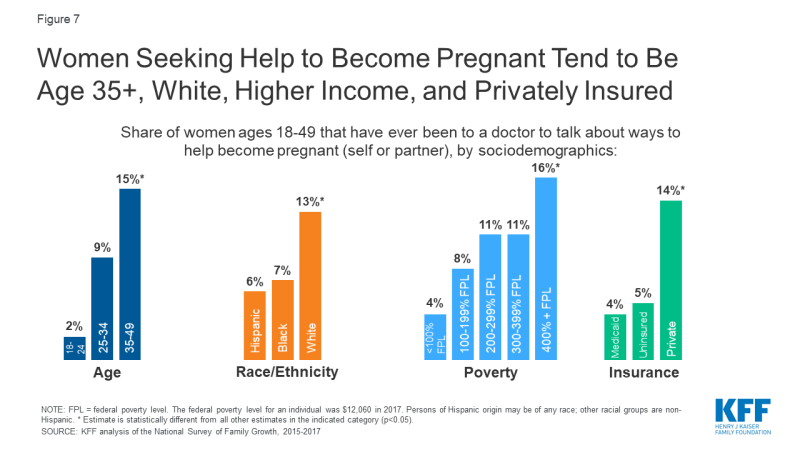
Figure vii: Women Seeking Help to Become Pregnant Tend to Be Age 35+, White, Higher Income, and Privately Insured
Other research has found that use of fertility testing and treatment besides varies past race. An analysis of NSFG data institute that amid women who reported using medical services to aid go meaning, similar shares of Blackness (69%), Hispanic (70%) and White (75%) women received fertility advice. However, less than half (47%) of Black and Hispanic women who used medical services to become pregnant reported receiving infertility testing, compared to 62% of White women, and even fewer women of colour received treatment services. According to an assay of surveillance data of IVF services, employ is highest among Asian and White women and lowest amidst American Indian / Alaska Native (AI/AN) women. Racial inequities may exist for fertility preservation as well; a study of female patients in NY with cancer found disproportionately fewer Blackness and Hispanic patents utilized egg cryopreservation compared to White patients. On average, more Black, Hispanic, and AI/AN people alive below the federal poverty level than people who are White or of Asian/Pacific Islander descent. The high cost and limited coverage of infertility services make this care inaccessible to many people of color who may desire fertility preservation, but are unable to beget it.
Iatrogenic Infertility
Iatrogenic, or medically induced, infertility refers to when a person becomes infertile due to a medical procedure done to treat another problem, most often chemotherapy or radiation for cancer. In these situations, persons of reproductive age may desire future fertility, and may opt to freeze their eggs or sperm (cryopreservation) for subsequently use. The American Social club for Reproductive Medicine (ASRM) encourages clinicians to inform patients about fertility preservation options prior to undergoing handling likely to cause iatrogenic infertility.
Withal, the toll of egg or sperm retrieval and subsequent cryopreservation can exist prohibitive, peculiarly if in the absence of insurance coverage. Only a scattering of states (CT, DE, IL, Dr., NH, NJ, NY, and RI) specifically require private insurers to cover fertility preservation in cases of iatrogenic infertility. No states currently require fertility preservation in their Medicaid plans.
LGBTQ populations
LGBTQ people may confront heightened barriers to fertility care, and discrimination based on their gender identity or sexual orientation. Section 1557 of the Affordable Intendance Deed (ACA) prohibits discrimination in the health care sector based on sex, only the Trump Administration has eliminated these protections through regulatory changes. Without the explicit protections that have been dropped in the electric current rules, LGBTQ patients may be denied wellness care, including fertility care, nether religious freedom laws and proposed changes to the ACA. Even so, these changes are being challenged in the courts because they conflict with a recent Supreme Court decision stating that federal civil rights law prohibits discrimination based on sexual orientation and gender identity.
In a commission opinion, ASRM concluded information technology is the upstanding duty of fertility programs to treat gay and lesbian couples and transgender persons, equally to heterosexual married couples. They write that assisted reproductive therapy should not exist restricted based on sexual orientation or gender identity, and that fertility preservation should be offered to transgender people before gender transitions. This allows transgender individuals the ability to have biological children in the future if desired. Despite this recommendation, in same states with mandated fertility preservation coverage for iatrogenic infertility, it remains unclear if this benefit extends to transgender individuals, whose gender affirming care can event in infertility. Additionally, many state laws regarding mandates for infertility handling contain stipulations that may exclude LGBTQ patients. For example, in Arkansas, Hawaii and Texas and at the VA, IVF services must use the couple's own eggs and sperm (rather than a donor), effectively excluding same sex activity couples. In other states, same-sex couples do non meet the definition of infertility, and thus may not qualify for these services. Data are defective to fully capture the share of LGBTQ individuals who may utilize fertility assistance services. Enquiry studies on family building are frequently non designed to include LGBTQ respondents' fertility needs.
Unmarried Parents
Unmarried persons are often excluded from access to infertility treatment. For example, the same IVF laws cited above that crave the couple's own sperm and egg, effectively exclude single individuals too, as they cannot use donors. Some grants and other financing options besides stipulate funds must go towards a married couple, excluding single and unmarried individuals. This is in opposition to the ASRM committee opinion, which states that fertility programs should offer their services to single parents and unmarried couples, without discrimination based on marital status.
Looking Forward
On a federal level, efforts to pass legislation to require insurers to comprehend fertility services are largely stalled. The proposed Access to Infertility Treatment and Care Human activity (HR 2803 and S 1461), which would require all wellness plans offered on group and individual markets (including Medicaid, EHBP, TRICARE, VA) to provide infertility treatment, is nevertheless in committee (and never made it out of committee when proposed during the 115th congress). There has been some more movement on the state level. Some states require private insurers to cover infertility services, the nearly recent of which was NH in 2020. Currently, NY continues to be the first and but state Medicaid programme to encompass any fertility treatment.
For those who desire to take children, obtaining fertility intendance can be a stressful process. Stigma around infertility, intensive and sometimes long or painful handling regimens, and uncertainty about success can accept a toll. On top of that, in the absence of insurance coverage, infertility care is cost prohibitive for most, particularly for depression-income people and for more expensive services, like IVF or fertility preservation. Meaning disparities be within access to infertility services across, dictated by state of residence, insurance programme, income level, race/ethnicity, sexual orientation and gender identity. Achieving greater disinterestedness in access to fertility care will likely depend on addressing the needs faced past depression-income persons, people of color and LGBTQ persons in fertility policy and coverage.
What Male Reproductive Services Are Covered By Health Insurance,
Source: https://www.kff.org/womens-health-policy/issue-brief/coverage-and-use-of-fertility-services-in-the-u-s/
Posted by: dickersonloste1954.blogspot.com


0 Response to "What Male Reproductive Services Are Covered By Health Insurance"
Post a Comment